Take more liquids during the day. Shift times for drinking. Increase fluid intake earlier in the day and reduce it later in the evenings which could result less wet bed.
Schedule bathroom breaks. Regular urination schedules every two to three hours and right before bedtime is good option that’s helpful treatment for how to stop bedwetting.
Don’t take any caffeinated products before sleeping. Caffeine acts as a diuretic, meaning that it simulates the bladder to produce more urine. Caffeinated drinks include tea, coffee, colas, energy drinks, etc. should be avoided before you go to sleep.
Constipation can result in bed wetting. Consider if constipation is a factor. Because the rectum is right behind the bladder, difficulties with constipation can present themselves as a bladder problem, especially at night. This affects about one third of bedwetters who wet the bed.
Performing bladder exercises. Thebladder exercises can help you to know how to stop bedwetting and help to hold the urine for a little longer prior to using the bathroom; this will help strengthen bladder control over time. Do take medical advice before practicing such types of exercises.
Medication for bedwetting. Doctors might suggest medication if you want an answer for how to stop bed wetting but one must remember that bedwetting medication has its side effects, its essential to discuss these options with your doctor prior to making a decision.
Don’t blame a bedwetter. Bedwetting is no one’s fault. No one wants to wake up to a wet bed. Blaming won’t help stop wetting the bed. It might only worsen the situation.
Use incontinence supplies. There is a large variety of waterproof bed pads designed to cater to bedwetter. These waterproof beddings are highly absorbent and not only protect your bed but they could lead to a more comfortable sleep.
Keep a stain remover handy. Keeping a stain and odor remover handy is always a good option. Get a stain remover that solves the purpose so you need not to sleep on the bed that smells of urine.
Cut down on alcohol. For adult bedwetter he must try to cut down on alcohol and caffeinated products before sleeping.
Try adult diapers. Get diapers specially designed for adults. Use of these absorbent briefs during the night keep your bed safe if there is any bedwetting accident. If you need help deciding an absorbent brief you can reach one of our specialists to assist you better.







 Our #1 Top SellerIdeal for Daily Use
Our #1 Top SellerIdeal for Daily Use Premium Quality BeddingSoft and Comfortable
Premium Quality BeddingSoft and Comfortable Premium Quality BeddingLarge Urine Absorption
Premium Quality BeddingLarge Urine Absorption AFFORDABLE PRICECHANGE DAILY AS NEEDED
AFFORDABLE PRICECHANGE DAILY AS NEEDED
 Sleek, Stylish and Affordable Watch
Sleek, Stylish and Affordable Watch Multi-Function Watch with Numerous Features
Multi-Function Watch with Numerous Features Recommended watch for teens and adults
Recommended watch for teens and adults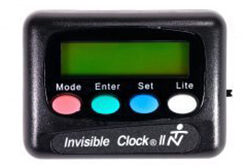 Perfect for medication and other reminders
Perfect for medication and other reminders



























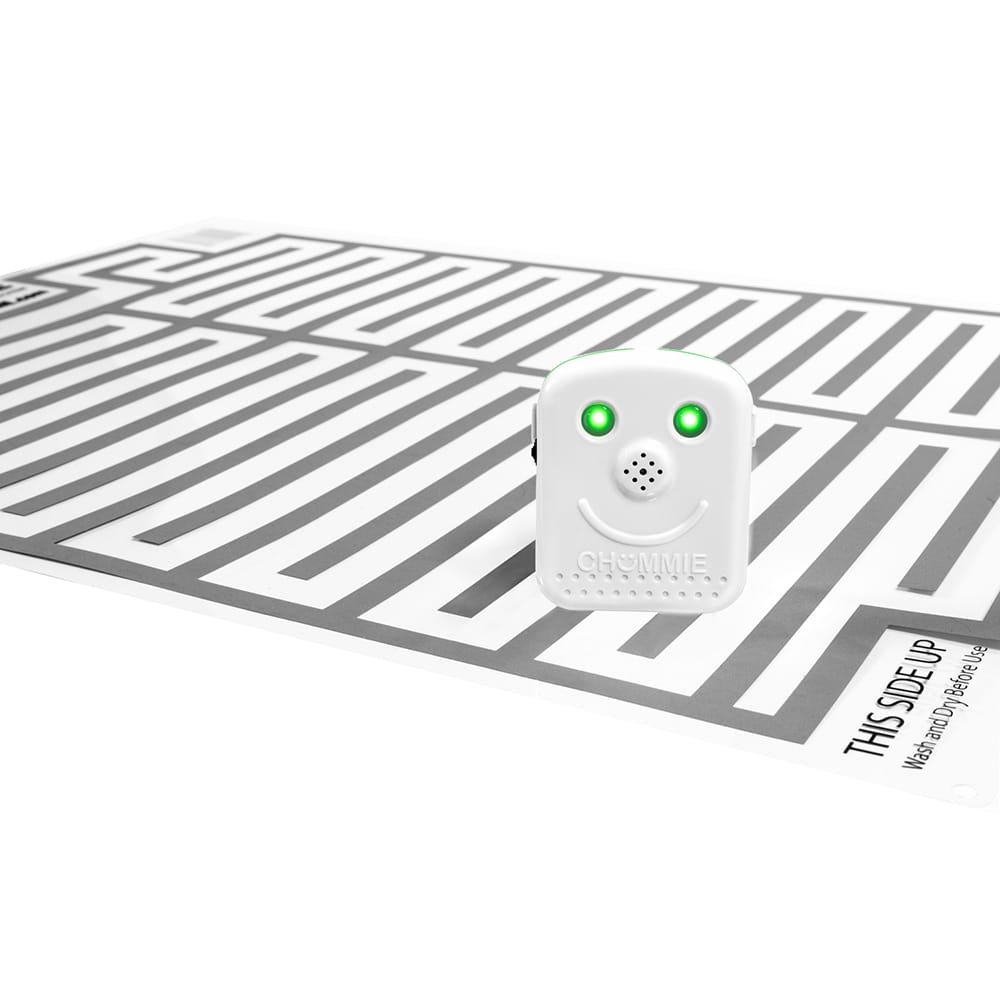
 Children
Children Play Alert Tones
Play Alert Tones Why buy from us
Why buy from us LARGE SELECTION
LARGE SELECTION EFFECTIVE ALARMS
EFFECTIVE ALARMS FAST SHIPPING
FAST SHIPPING SPECIALIST SUPPORT
SPECIALIST SUPPORT